After five years of thinking and consultation among all stakeholders, we all still freak out when finally the government introduces a series of long-thought-out changes to the MBS. What is wrong with this picture?
A couple of stats on this week’s rant that become relevant as you read on:
- Medical error is the third-leading cause of death in the US, accounting for 250,000 deaths every year
- It’s estimated that there are at least 49 deaths per day and 139 permanent injuries created by medical error in Australia
- You are 100 times more likely to die from a medical error than a car accident in Australia
Another way of putting the above stats is that healthcare crashes the equivalent of one A380 Airbus every day around the world.
Such comparisons have led to some pretty funny articles on the topic of “If we ran airlines like we ran healthcare”.
Here’s one assessment of what such a situation might look like, from Dr Joel Zivot, a US anaesthesiologist writing last year for the US medical daily Medpage Today:
- Passengers would struggle to only fly on planes that had pilots whom they had heard of before.
- Pilots would fight with each other, sometimes in front of passengers.
- When the plane landed, the pilot would be the first to exit the plane and would not address passengers as they left the plane.
- Pilots would demand special equipment for particular planes that they would fly and would fly only on specific planes that stocked the equipment in question.
- During certain times of year, no flights would be available, as pilots would be attending special meetings.
- Pilots would offer special seats and reduced fares to personal friends or famous passengers.
- On a daily basis, flight arrivals and departures would be frequently incorrect. Sometimes passengers would be asked to arrive many hours before flights, not be permitted to eat while waiting, and then have the flight cancelled without warning or explanation.
- Pilots would not follow standard operating procedures and instead conduct themselves in any fashion that they believed to be correct. No one would challenge them.
- Pilots could fly for 36 hours straight with no relief.
- Pilot trainees, sometimes with very little experience, and with very little supervision, would fly planes. Passengers would have no knowledge of this.
- Senior pilots would berate pilots in training, occasionally in front of passengers.
- Senior pilots would demand the most favourable take-off and landing priorities.
- Passengers would be required to wait on planes until the pilot arrived.
- The price of tickets would be unknowable at the time of ticket purchase and would be subject to change without warning. Passengers would receive bills in the mail for weeks or months after the flight. It would be very difficult for passengers to get information on the particulars of fees. Sometimes if a passenger complained, the fee would be reduced.
- Individuals dressed as pilots with minor differences to the pilot uniform would sit in the cockpit and sell pilots new features on the aircraft while the aircraft was flying.
Dr Zivot’s original article is HERE (another good one from The Atlantic is HERE)
When the news cycle started this week on MBS changes, it was pretty obvious that the major news networks were getting some of their material from lobby groups.
One item on a commercial network featured a former Olympian complaining that they had to undergo a lot of surgery in their life, both prior to their appearing in the news item, and a lot into the future. This poor soul was desperately worried that the changes were going to affect them, but even more worried about the general public.
Everyone was getting in on the act or predicting the changes might be bad, but no one actually had a clue what the changes would actually mean.
The Medical Republic even published an analysis piece from The Conversation by Stephen Duckett, titled MBS changes could leave patients with higher gap fees, in which Duckett pointed out that because of the number of changes and the complexity of the relationship of the changes to how the private health system works out its rebates, it might take some time to work out if patients were actually better off.
The intent of the changes to the MBS isn’t just about patients being better off, though. They are about system efficiency and value. It’s about money.
As technology and medical knowledge changes, so should the system of reimbursement for those changes. We shouldn’t be funding out of date procedures or incentivising inefficient procedures.
Duckett points out that the MBS should be subject to constant ongoing review and change.
But these changes are the culmination of a review started more than five years ago now, after virtually no updates had been made to the MBS over 30 years.
No wonder people are freaking out. It’s a lot of change in a short amount of time and no one likes change, especially in healthcare because when you change stuff in healthcare there has to be a loser usually somewhere in the value chain.
Traditionally if surgeons, cardiologists or anaesthetists have looked like they were going to be on the losing side, politics kicked in, and often the AMA too, and nothing changed. Does anyone remember how powerful Dr Bruce Shepherd once was in the politics of Australian medicine?
When Professor Bruce Robertson, MBS Review Committee chair, mentioned during a talk to the practice owners conference of the RACGP in 2019 that some of the anaesthetic items were outdated and probably being overused (rorted?), the powerful Australian Society of Anaesthetists demanded Robertson’s resignation from the health minister the next day.
The AMA came out saying it had patients’ best interests at heart by expressing concern about the MBS changes this week . We gather the potential affect on their member cardios and surgeons income stream didn’t enter their minds.
Like most stakeholders, the AMA has a degree of conflict in how they present the situation. And like most stakeholders, when you tinker even a little with Medicare, everyone becomes nervous.
In a related event, when Health Minister Greg Hunt did one of his “look at the bulk-billing scoreboard” press releases this week, RACGP president Dr Karen Price (along with an army of social media enabled doctors) responded. Her tweet is below and an article addressing the premise of the tweet is featured in the college information service, newsGP (HERE).
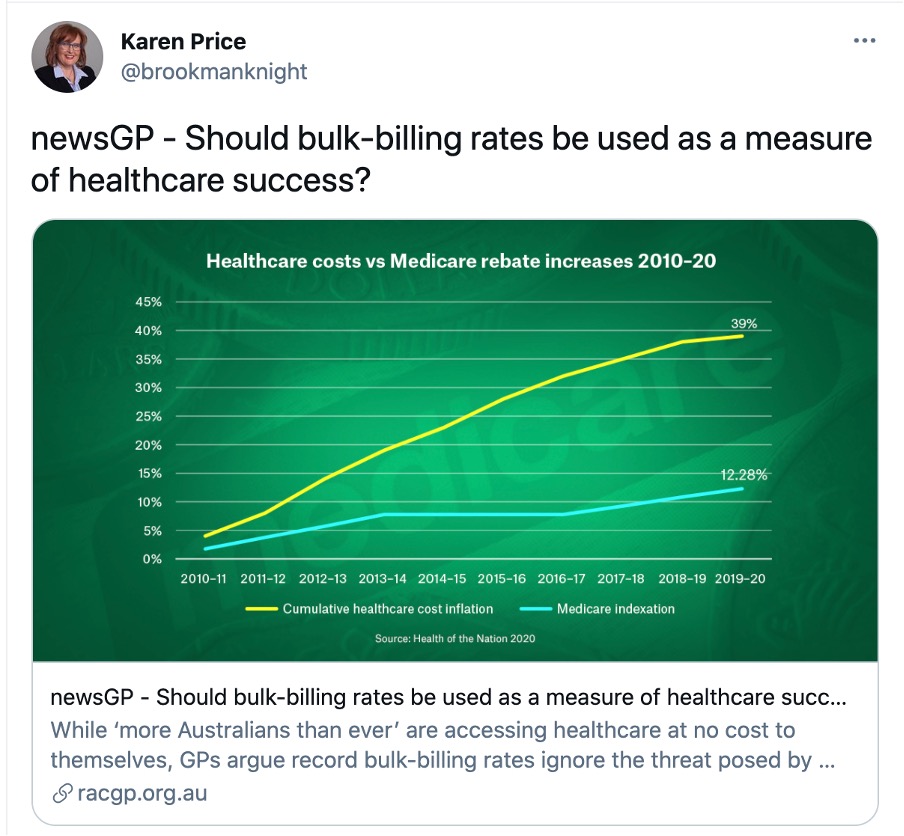
The newsGP article is only slightly less rambling than this oped, so to save you some time, here are Dr Price’s money quotes:
“When did the bulk-billing rate become the measuring stick for optimal health and wellbeing?”
And for context:
“The economics of an unsupported health system and its clinicians are far more costly to patients and to taxpayers. I look forward to continued investment and reform where it matters most”.
The other item related to both the above, and the MBS changes (with all the accompanying confusion), was the release by the AMA of its vision for Australia’s health, which is HERE.
We aim to serve at TMR, and recognising that we will often waste chunks of your precious time with rants such as this one, we try to make up for it where we can with concise executive summaries of important new documents that come to light, such as this one summarising the AMA’s new vision for Healthcare here:
GPs are hopelessly paid and underutilised in a system that everyone knows is marching to a chronic care crisis where we need them more than ever, hospitals are very expensive and less and less effective so we need to get smarter all around or we won’t be able to afford them much longer, private healthcare is a mess, dying a slow death and not helping anyone but prosthetics manufacturers and private hospital operators, but politically it has to be made part of the equation somehow, we should empower patients, and technology would help if we could just organise a bit better.
Here it is in icons: I left out the last icon in the exec summary because I didn’t quite understand what it meant…
I’m not sure that the AMA is going to be happy with that executive summary.
As a vision document it’s actually a pretty good summary of the issues and what we should be thinking about more carefully. And kudos to the AMA for putting GPs front and centre of the document, even if it’s entirely obvious they need to. It must have been difficult to order the icons overall, but that patients got relegated to No 4 position in the list is possibly a worry.
But I don’t think understanding the issues, the politics, the component parts and their relative importance and positioning is the issue here. If you read the RACGP vision statement, it’s pretty similar: All problems, no solution.
And by solution we aren’t talking the banal stuff such as “pay GPs more” and things will magically get much better. They probably won’t if that’s all you do. Things might even get worse if you paid GPs better without a framework in which you can change the whole system in some sort of alignment.
Dr Price of the RACGP is, in reply to Minister Hunt, correctly suggesting that you can’t measure value of the money invested in healthcare system by a “bulk-billing scoreboard”.
But it’s a pretty sure bet you couldn’t do it either by measuring it simply by investing more in the clinicians that matter most in our future health system, GPs, which is where she was going in her article and tweet.
The system is an inordinately complex milieu of risk, regulation, information asymmetry between the system and consumers, money, politics, governance and emotion (life and death). Measuring value of investment in a system like this is necessarily going to be a complex algorithm.
It’s not like anyone is getting particularly right anywhere in the world either, although some more manageable smaller population groups in Scandinavia and parts of Eastern Europe appear to give it a good go these days.
To return to our travel and flying analogy, we see that this industry, with similar attributes (not all similar I know, but look at the list two pars above and there is a lot going on in air travel that is going on in healthcare) isn’t crashing one A380 per week at all.
In fact, when two 737 MAX airliners go down in the space of one year, all hell breaks loose, there is havoc globally in the whole industry, fear and loathing among consumers, and years of creep reveal the system has failed substantively for the first time in decades, and needs to be upgraded significantly.
What is healthcare missing and why?
Why do we care a lot more about when an airliner crashes – and have a mechanism to address the issue reasonably quickly – when we are crashing one big airline per day in healthcare, but no one can seem to harness the system and those in it to bring this appalling statistic under a bit more control?
What might bind all elements of our healthcare system in a manner that the airline industry and all who fly in her have become bound in a meaningful way over time, to global standards of safety and care?
The answer obviously isn’t simple or we would have started already moving towards it, and the analogy made here between the two industry sectors is oversimplified in various aspects. It’s a technique to try to unravel some basics.
One aspect of the issue, and something that possibly does span the entire system as a theme that needs to be understood and standardised as a starting point of value for all system stakeholders, is: “What is the value of a life?”
If you look at most modern doctor indemnity policies, the answer is about $20 million. But that’s just one stakeholder. There are lots of other stakeholders who need to be satisfied.
Another possibly important universal aspect, which is being examined by a group of doctors in Australia today, some politicians and policy makers, and which has been mentioned above in the context of the how the airline industry found its way to a safer system, is “standards”.
Why doesn’t medicine have “standards” that are constantly reviewed and agreed upon by the most important stakeholder bodies regularly, including patient stakeholders? Just about every other industry sector does.
As wicked as this problem sounds, there are a lot of people thinking about it and some very senior healthcare leaders think there are some reasons to believe there is a way to navigate through to a better system.
But it’s going to take agreement on some of the basics among the leading stakeholder groups on concepts like the cost of a single life, ‘value’ and ‘global standards’ which consider not just the clinical dimension, but the ethical dimension of the value of life and well being.
More next week.


