Advanced trainees Dr Bonnia Liu and Dr Elaine Ng present their takes on the ARA ASM.
Advanced trainees Dr Bonnia Liu and Dr Elaine Ng present their takes on the ARA ASM.
Dr Bonnia Liu
The second year running of a hybrid format for the Australian Rheumatology Association Annual Scientific Meeting has provided, in my opinion, a well-rounded coverage of topical issues spanning advances in basic science and new treatment options to the broader issue of healthcare access, workforce shortages and trainee selection in rheumatology.
The clinical ground rounds cannot be missed this year, filled to the brim as they are with some fascinating cases to tickle those little grey cells. But I shall not include any spoilers for those who want to watch the recorded sessions. For now, I will focus on a few sessions that sparked particular interest to me.
I started off on Saturday morning with a soy latte, a ham-and-cheese croissant and an extremely thorough and informative overview of our evolving understanding of immune-mediated myositis (Concurrent Session 5A: NAM and Clinical Pearls, Associate Professor Lisa Christopher-Stine).
Professor Christopher-Stine addressed the traditional grouping of similar but heterogeneous conditions under the umbrella term of “polymyositis”, meaning simply “inflammation of muscles”. But over the past decade we have achieved so much more in the understanding of myositis pathogenesis that perhaps we need to start being more specific.
Advances in autoantibody detection and correlation with specific histopathological and clinical features have been the key to identifying homogenous clinical cohorts to allow better understanding of disease prognosis and response to treatment.
The highlight of the talk was the clarification of the clinical distinction between immune mediated necrotising myopathy (or necrotising autoimmune myositis), specifically anti-HMGCAR autoantibody-positive myopathy, and anti-SRP autoantibody-positive myopathy. Also addressed was how to differentiate these from the more benign presentation of statin-induced myopathy.
After morning tea, Professor Seza Özen (Concurrent Session 6A: Autoinflammation/monogenic lupus) explored the spectrum of autoinflammatory and autoimmune diseases, with an overview of the alphabet soup of interferonopathies.
Catchy acronyms aside (CANDLE Syndrome, we’re looking at you), the discovery and identification of specific genetic mutations and characterising clinical phenotypes provided us with greater understanding regarding the pathogenesis of autoimmunity as a consequence of defects in central and peripheral immune tolerance.
Following this, Dr Andrew McLean-Tooke outlined multiple syndromes arising from monogenic mutations that overlap with clinical features of systemic lupus erythematosus (SLE), and suggested that patients with early-onset manifestations and a strong family history of autoimmune diseases might benefit from genetic screening.
It is not possible to manage autoimmune diseases in isolation without knowing about the immune cells involved, and time and time again, we find ourselves working with our haematology colleagues to develop new treatment options for our rheumatology patients.
After the historical success of “borrowing” cyclophosphamide, methotrexate and rituximab from the haematologists, what else is new?
Professor Georg Schett (Concurrent Session 8B: CAR T cell therapy for autoimmunity – is it feasible and what can we expect?) described the potential of chimeric antigen receptor (CAR)-modified T cells in the treatment of severe refractory SLE. CAR T cell therapy has been all the rage in the haematology world for the treatment of aggressive lymphomas and involves modifying a patient’s own T cells to target specific cell types in the body. In the case of SLE, CAR T cell targeted at CD19+ B cells demonstrated clinical and serological remission for a small group of patients.
Another area in need of new therapies is diffuse systemic sclerosis.
An emerging haematology-based therapy discussed this weekend was autologous haematopoietic stem cell transplantation (AHSCT) for severe systemic sclerosis by Dr Ross Penglase (Concurrent Session 9B: Autologous Haematopoietic Stem Cell Transplantation for Severe Systemic Sclerosis Using Standard Dose Cyclophosphamide Conditioning – A Single Centre Experience).
This clinical trial has demonstrated improved parameters including survival outcomes, skin score, physical outcomes and lung function. Currently, symptom management has been the main goal of treatment for our patients with diffuse systemic sclerosis, with few options available to prevent disease progression. Thus, we will be watching this space with interest and hope for our patients.
This short report does not do justice to the range of topics covered during the conference, but the benefit of hybrid sessions is that concurrent sessions are recorded for later viewing. Hello, weekend plans!
Dr Bonnia Liu is a rheumatology fellow and nuclear medicine advanced trainee at Austin Health in Melbourne.
Dr Elaine Ng

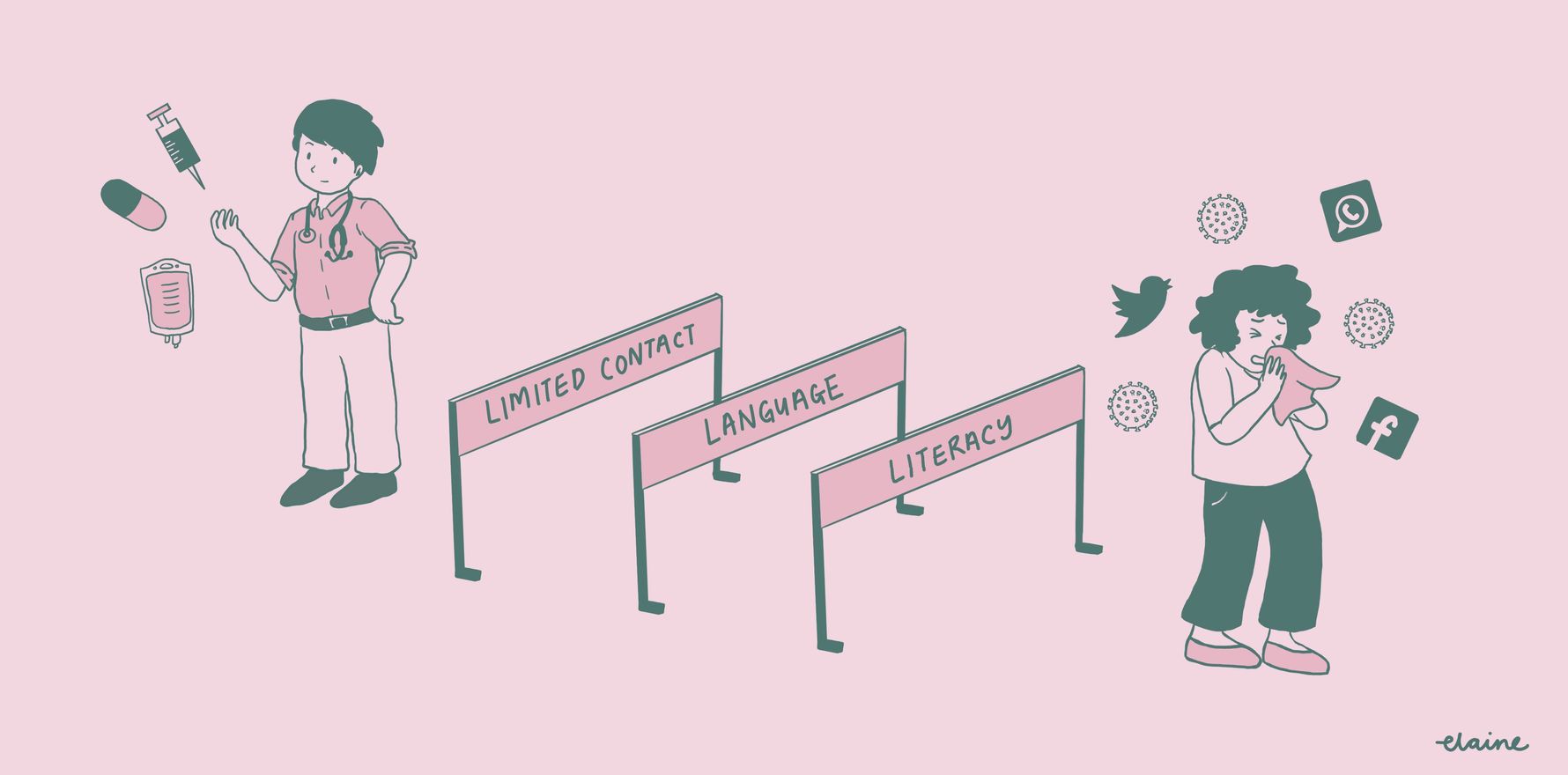
It is remarkable how rapidly covid research has moved from bench to bedside over the past 18 months. Although experts have highlighted the efficacy of vaccines and anti-viral treatment in the covid session, the common theme across the talks was the need for better information dissemination so our patients could better access available therapies.
Dr Elaine Ng is a rheumatology advanced trainee based in NSW who enjoys drawing.