MRI is used to investigate increasing lower-limb weakness in a 70-year-old following an L3/4 posterior fusion and discectomy.
A 70-year-old female presented with increasing lower-limb weakness, particularly on the left.
This was following an L3/4 posterior fusion and discectomy, during which it was noted an intraoperative small dural tear was sustained along with a cerebrospinal fluid leak.
An MRI was ordered to investigate whether there was the presence of neural compression.
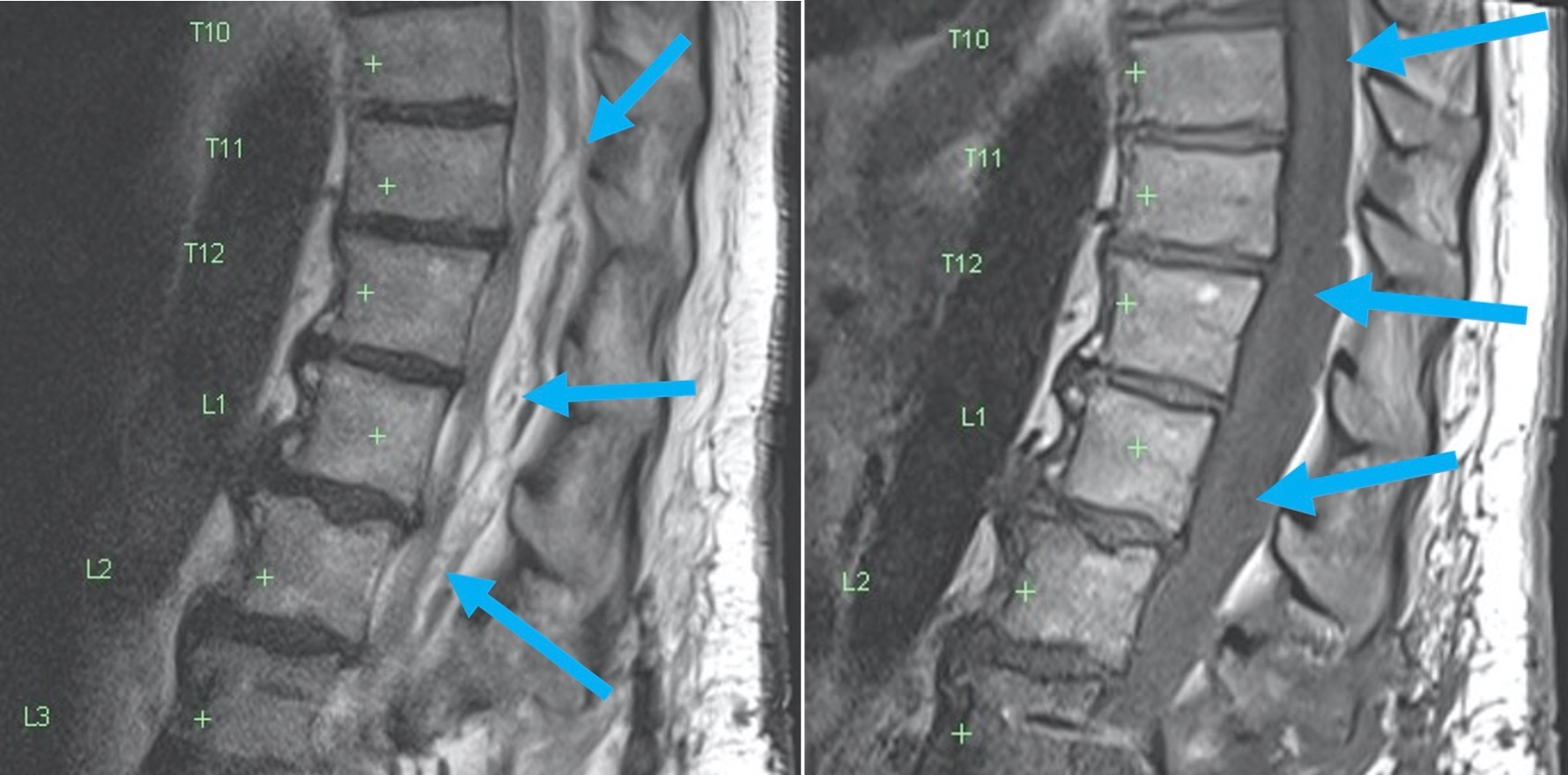
On MRI, there is the presence of extensive T2 heterogeneous high signal and T1 low signal, which was of similar signal characteristics to fluid in the epidural space posteriorly, extending rostrally from the operative site at L3/4 into the thoracic spine. This appeared to exert mass effect on the adjacent cord, displacing it anteriorly and distorting the thecal sac. There is no cord T2 high signal to suggest cord myelopathy.
Given the history of CSF leak, this could at first glance be assumed to represent a CSF collection/pseudomeningocele. However, on closer inspection of the axial T2 images, there are fluid-fluid levels, with markedly hypointense (dark) material layering in the dependent (dorsal) portions, and bright signal in the non-dependent (ventral) portions. The low signal layering probably indicates the presence of blood mixed with fluid either from the CSF leak or from evolving liquefying blood. In addition, there are internal septations within this fluid-like collection.
Typically, extradural CSF leaks tend to follow water signal on all MRI sequences (homogeneously low signal T1, high signal T2), are not septated, do not exhibit fluid-fluid levels, and do not exert mass effect on the cord or cord compression.
The presence of this low T2 signal, coupled with the history, helps to derive the diagnosis of an epidural haematoma. The patient returned to the operating theatre for further management and evacuation.
Fig A: Sagittal T2 image showing prominent T2 bright material posterior to the cord arising from the operative site and propagating superiorly, resulting in cord compression (blue arrows)

.
Fig B: Sag T1 image demonstrating that this material is similar to CSF in its intensity – the haematoma is indicated by the blue arrows; CSF is indicated by the red arrows

.
Fig C 1 &2: Axial T2 image showing heterogeneous low signal layering at the dependent portion/dorsal part of the collection (blue arrows) indicating blood, and displacement of the cord (yellow arrow). Note the septations in the collection (red arrow). There is no CSF remaining around the cord (orange arrow).


Dr Sebastian Fung is a musculoskeletal radiologist who undertook an MRI imaging fellowship in Hospital for Special Surgery in New York. He now works in Sydney at St Vincent’s Private Hospital and Mater Hospital.