The RACP is betting the house that the new curriculum will lead to significant cultural change and address the ‘failure to fail’.
There will be significant changes to how future rheumatologists learn, are assessed and progress through the advanced training program. Find out what to expect when the new curriculum comes into effect in 2026.
Speaking to delegates at the ARA ASM in Adelaide earlier this month, Dr Narainraj Kamalaraj, chair of the RACP’s rheumatology advanced training committee, highlighted how changes to the advanced training program’s curriculum would have a huge impact on trainees.
“The changes are happening in four key areas [standards, progression, learning and assessment and technology], and I would say the biggest and most important sections to pay attention to are the learning and assessment and progression sections,” the senior staff specialist at Campbelltown and Camden hospitals said.
“In a nutshell, we need to move towards a far more modern, pragmatic approach to assessment.”
Dr Kamalaraj told delegates that early, timely and authentic feedback was critical to the new training program.
“This is where the cultural shift has to come in, because the biggest danger that I keep hearing about as the chair of the ATS is that trainees who are not yet meeting the standard that they need to progress are not being identified [early enough], or it’s not being made explicit [that they’re struggling]. We are trying to mitigate this risk, [but] it’s going to take more than the curriculum document to do that,” he said.
“We have a stewardship and responsibility as supervisors not to kick it down the road, but to actually give the feedback that is authentic and relevant early in training so that trainees can get the support they need. The stigma around training and support needs to end with us.”
The specific learning goals of the training program are divided into three categories: be, do and know.
Related
The “be” category refers to standardised professional behaviours that will be consistent across all medical specialties, while the latter two categories relate to being able to perform certain tasks and understand the theoretical content expected of a rheumatologist.
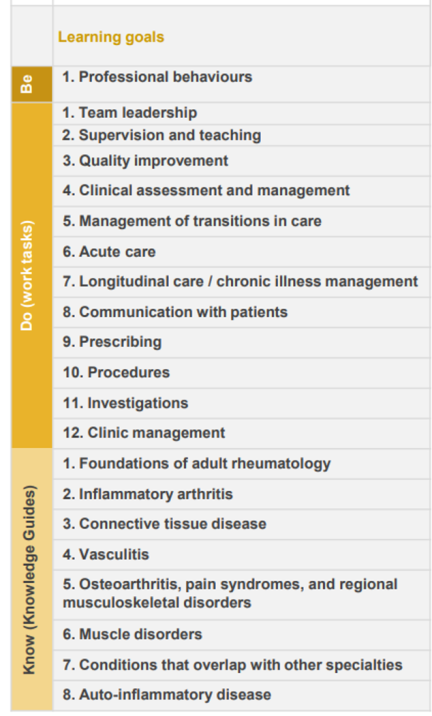
Dr Kamalaraj explained that the curriculum review group tried to keep the learning goals as broad as possible to allow for any changes that might occur with medications and even disease, meaning the curriculum’s content can remain relevant for a longer period of time, before stressing the importance of becoming familiar with the learning goals once the training documentation is finalised and released.
“Everything we do as supervisors, and everything the trainees will do as learners, will be mapped to these learning goals. These are the goals that need to be achieved by the end of the training program,” he said.
Trainees will be required to develop one learning plan per rotation in conjunction with their supervisor(s) under the new program. Logbooks will still be required; one for the cases managed by the trainee and the other for the procedures undertaken by the trainee.
Supervisors will be required to submit four progress reports over the course of each rotation, moving away from simple yes/no responses to a more detailed and structured assessment of the trainee’s performance.
Non-physician staff will be able to provide feedback on trainees via observation captures in the new online system that will house the training program – provided the trainee grants them access to do so.
This may pose potential challenges as it creates selection bias about who can provide written feedback about the trainee and means that staff not given access to the online system will be required to speak to the supervisor about the trainee. The latter point again hinges on staff members being willing to provide direct, explicit feedback.
The proposed learning, teaching and assessment structure during advanced training will be split into three phases. Progression between the phases will be based more on the competence of the trainee – as assessed by an independent panel, not the direct supervisor – rather than trainees spending 12 months in each phase.

Dr Kamalaraj acknowledged the new structure raised questions, such as how it would be accommodated in time and resource-limited settings for trainees who may require additional assistance. He conceded that this was an area the RACP had not been able to address and that they had been directed to make these changes by the Australian Medical Council.
Trainees will also be required to complete a larger number of learning courses that will be common across different specialties as part of the new program.
Currently, trainees are only required to complete a course on Australian Aboriginal, Torres Strait Islander and Mãori competence and cultural safety. Under the new program, trainees will also need to complete the college’s advanced training orientation, a health policy, systems and advocacy course and the supervisor professional development program.
“Learning how to be supervisors themselves is a good idea, as it helps them promote their feedback literacy,” said Dr Kamalaraj.
However, requirements around attending conferences have been loosened. The new program requires trainees to attend at least one ARA Annual Scientific Meeting during the course of the program (but recommends attending each year if possible) and recommends they present (either a poster or a talk) at one national or international conference during the same timeframe.
Further details on the proposed changes to the adult rheumatology training program are available online.
ARA 25 was held at the Adelaide Convention Centre from 3-6 May.